At least 6.7 million children are at high risk of becoming uninsured for some period of time, according to new research from the Georgetown University Center for Children and Families, a W.K. Kellogg Foundation (WKKF) grantee.
About half of all children in the United States, nearly 40 million kids, are currently insured through Medicaid and/or the Children’s Health Insurance Program (CHIP), which offers health insurance to children in low-wealth families. Throughout the COVID-19 pandemic, children covered under Medicaid and CHIP had stability in their healthcare coverage, thanks to continuous coverage requirements included in Congress’ coronavirus relief bills. But, the protections are likely to expire this year, perhaps as early as this summer.
When those protections expire, states are required to re-evaluate the eligibility of all Medicaid recipients, including children. The outcomes will vary enormously for children depending on where they live and how well their states handle the transition. Children in some states – including Florida, Georgia, Missouri, and Texas – are at particularly high risk for losing coverage because of the way those states administer their Medicaid programs.
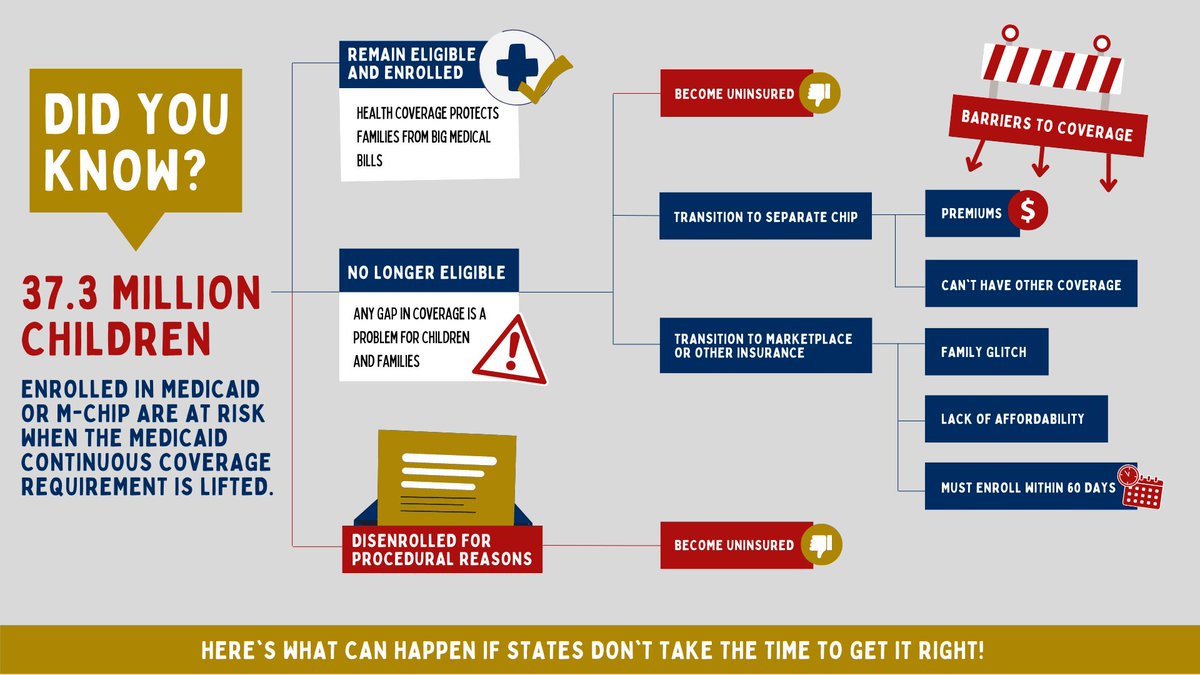
What Can Happen if States Don’t Take the Time to Get it Right?
This infographic from Georgetown University Center for Children and Families breaks down what happens if states don’t take the time to get it right. In short, it means that millions of children could be disenrolled for procedural reasons – like expired contact information, incomplete renewal forms, etc. – and become uninsured.
What Actions Can Community Members Take to Minimize Procedural Disenrollment?
Update Your Contact Information
- Make sure your state Medicaid has your current mailing address, phone number, email, or other contact information. This way, they’ll be able to contact you about your Medicaid or CHIP coverage.
Check Your Mail
- Your state Medicaid will mail you a letter about your Medicaid or CHIP coverage. This letter will also let you know if you need to complete a renewal form to see if you still qualify for Medicaid or CHIP.
Complete Your Renewal Form
- Fill out the form and return it right away to help avoid a gap in your Medicaid or CHIP coverage.
Advocate to Ensure that Families Are Reached, Where They Are
- Work with state Medicaid to ensure that they are using culturally and linguistically appropriate outreach and communication to reach families where they are. Check out this toolkit from the Centers for Medicaid and Medicare Services in the U.S. Department of Health and Human Services!

What Actions Can State and Federal Policy Makers Take To Minimize Procedural Disenrollment?
Georgetown University Center for Children and Families suggests that state and federal policymakers could take the following actions to minimize procedural disenrollments in Medicaid and CHIP:
- Improve automatic renewal rates
- Boost eligibility and call center workforce capacity
- Increase funding for community-based outreach and application assistance, such as navigators and community health workers
- Send follow-up notices and reminders when action is required
- Maximize use of communication modes (mail, phone, automated messages, online accounts, text, email)
- Expand the ways enrollees can submit needed information either verbally or electronically to replace the inefficiency of processing paper documentation
- Work with Medicaid managed care organizations (MCOs) and health care providers to update contact information and remind members that their renewal is due
- Ensure that call centers have adequate, trained staff to avoid call wait times that impede families from getting assistance





Comments